The more you know about painful sex
Painful sex in the South Asian diaspora is way more common that it should be
Welcome to Brown Bodies: The more you know, a monthly educational series written with the help of amazing experts in their fields. This month we’re looking at painful sex.
I recently read an article that said South Asian women’s pain around sex is probably underdiagnosed, or not properly diagnosed, due to the stigma around sex, periods and tampons often held in South Asian communities. People are embarrassed to talk about it, think pain is normal or are ashamed that they’ve failed at sex. With the help of Dr Nitu Bajekal, one of my favourite gynaecologists —I know, not something I thought I’d ever say either — we’re going to try and change some of those misconceptions.
At 29, one kid in hand and another on the way, Dr Bajekal moved to the UK from India with the love of her life, Rajiv. They’d been at medical school together, him beginning to specialise in orthopaedics and her in obstetrics and gynaecology.
Now, with over 35 years worth of medical experience under her belt and having recently retired from the NHS, she is a consultant gynae, a surgeon, a women’s health specialist and an excellent TikToker. She’s a strong believer in access to healthcare and has made it her mission to create a ton of free resources — on her website, Instagram and TikTok — focused on education around female health like PCOS, endometriosis and menopause. She’s clear that she wants all of her work to ‘be inclusive to anyone assigned female at birth (AFAB) such as trans men and non-binary folk’.
Any of the advice in this piece applies to women and anyone assigned female at birth.
To make it easier to navigate this piece, these are the sections you can jump to:
First thing’s first
Why women don’t seek help
Getting to the root of the problem
Stop believing the myths
Reasons for painful sex
Psychological reasons for painful sex
First thing’s first
Anyone can be affected by painful sex.
Intercourse can be uncomfortable the first time, yes. Maybe a couple of times, at most. But, after that, it shouldn’t be an issue. Too many women are having painful sex, known as dyspareunia, without realising how big a problem that is and the knock on effect it has on things like confidence, relationships and pleasure.
It can happen at any age. The reasons it happens may be different for different age groups, but the symptoms and underlying conditions can often overlap.
Why women don’t seek help
Many women have put up with these symptoms and the poor quality of life it offers them for years without a diagnosis. Why? Well, why as a woman, especially as a South Asian woman, would you possibly expect to orgasm or actually enjoy sex? At the end of the day sex is your duty, right? No!
Women have a right to pleasureful, fun and pain free sex. As soon as we make it about duty, it’s no longer about a woman’s pleasure which is why so many don’t seek help — they’re just doing what they’ve been told is their job. That has to change.
With a partner, you don’t get into it because they don’t understand what you’re going through. The pain you have — from postpartum scars, the effects of postpartum blues, the effects of menopause, perimenopause, psychosexual dysfunctions or pelvic dysfunction you’re experiencing from your PCOS or endometriosis — is hard for them to empathise with. If they don’t know, you’ve got no one with you on your journey. No one to push you to seek help. Communicate your pain and its impact to your partner.
Finally, women don’t seek help because when they do, they’re repeatedly diagnosed incorrectly with thrush or vaginal infections or dismissed by doctors who say it’s normal.
Getting to the root of the problem
The first step to a proper diagnosis is to understand what you are experiencing, where you’re experiencing the pain and when it happens (is it just when you’re on your period, for example?). Girls and women are not equipped to advocate for themselves in the doctor’s surgery:
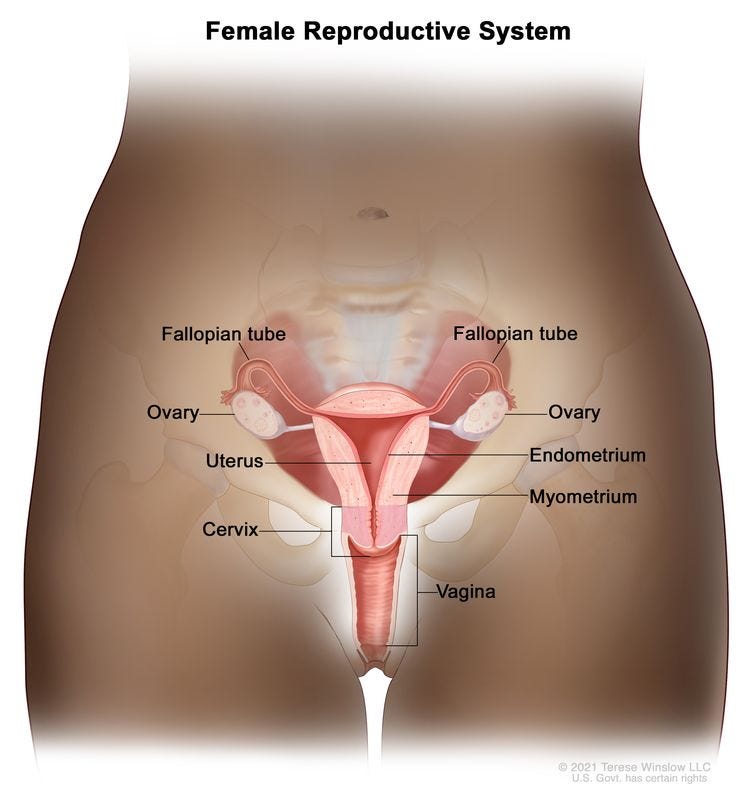
One in two women don't know where their cervix is.
One in four women don't know where their vagina is.
One in 10 women don't know where their reproductive organs are.
By shrouding our organs in shame, especially in the South Asian community, we’re not giving girls and women permission to talk openly and candidly about their own bodies. By not teaching our kids to call their genitals by their names — we call an arm an arm, so why do we call a vulva a vagina, nuni, fufu or ‘down there’? — our girls and, later on, our women can’t articulate what they are feeling and where exactly they’re feeling it. We’re doing them a huge disservice.
If you’re unable to express what is happening in your body, you’ll go to a time-pressed doctor, be quickly dismissed — you may be told to lose weight or to come back when you want to get pregnant, which has nothing to do with why you were there in the first place — and you’ll never want to seek help again.
You need to be able to say ‘I'm having painful sex’ and this is what I need help with. Or ‘Hey, I think this is stemming from endometriosis’ or another pelvic organic condition. Or ‘Sex is painful because it's superficial and I recognise it as eczema’ or other skin changes. You may even articulate that there is birth trauma, vulvodynia or tightness (more info down below!). Go in armed with information. Let the doctor know you mean business so it’s way less easy for them to fob you off:
When was your last period?
What’s your cycle like?
When does it hurt? Is it just during sex or other times too?
What medication are you on? Does pain happen when you take it?
If doctors haven’t looked for organic conditions that could be affecting you — pelvic inflammatory diseases, endometriosis, post birth traumas, for example — bring it to their attention before they can dismiss your pain as ‘something in your head’.
When people say ‘Oh don't go to Dr Google’ I ask, ‘Why not?’ Doctors go to Dr Google all the time. Just use information from reliable resources like the NHS website, Mayo Clinic, my website, The British Menopause Society, Verity (the PCOS charity) and The Daisy Network (for premature menopause and premature ovarian insufficiency).
An attentive doctor will take this into account. There are plenty of empathetic health professionals, sexual therapists, psychotherapists and doctors who want to help and will listen to you. They understand that chronic pain is little understood by the medical community. You may need to make repeated appointments so they know you're not going away but they’ll be there.
Stop believing the myths
It will get better over time.
You’ll get looser/less tight with more sex.
It will all sort itself out after childbirth.
Pain is to be expected.
Orgasms aren’t as important to women.
Pain is in your head so you need to get over it.
None of the above is true. If you’re in pain, get support.
Reasons for painful sex
There are two kinds of painful sex:
Superficial dyspareunia. This is the pain you get on initial penetration.
Deep dyspareunia. This is the pain you feel during deep penetration.
Causes can include:
Vaginal dryness
It can cause irritation, burning sensations, itchiness and pain. Some women complain of a sensation of paper cuts that may leave them sore for days.
It can happen at any age.
It can get worse during perimenopause and menopause.
Some women experience vaginal dryness while breastfeeding.
Some young women experience dryness when on the combined contraceptive pill.
You can get it if you’ve had your womb removed.
You may experience dryness if you’re having cancer treatments, such as chemotherapy.
It will happen if you’re not aroused, or aroused enough, during sex.
What can I do?
Avoid perfumed toiletries, feminine wipes, synthetic perfumes and soaps in the genital area — they increase dryness by removing natural body oils and beneficial bacteria.
Use non-biological laundry detergents which are low in harsh chemicals.
Use appropriate organic sanitary ware to manage your period like period pants, menstrual cups and discs and material pads.
You can apply natural oils such as coconut, Vitamin E or almond oil. Massage the vulval area with an oil after a shower to lock the moisture in. It’s totally OK and safe if some of the oil enters the vagina. Don’t use them with condoms though as they can degrade polyisoprene and latex. They can also act as natural spermicides so don’t use them when trying to conceive.
You can use a water-based vaginal moisturiser.
Using lubricants during intercourse can help.
Here are more general care tips.
If this doesn’t solve it, menopausal women and women who are breastfeeding may need local vaginal oestrogen and young women may want to consider a different form of contraception. Speak to your GP.
Vaginismus
Pain at the entrance of the vagina.
Why does it happen?
It depends. It may be because of a physical cause, vaginal spasms or tight vaginal muscles.
A doctor will want a detailed history to check that there is no previous sexual trauma which is causing you issues.
What can I do about it?
See a doctor about it.
Doctors, patients and partners — be patient. It often takes more than just a couple of consultations to get to successful, painless penetration.
If there is a partner, get them involved in understanding why you have vaginismus and what you will be doing to overcome it and how they can support.
In my experience, discussing the underlying causes alongside the use of graduated vaginal dilators — tubelike devices made of plastic or silicone that you put in your vagina to stretch your vaginal tissue — can help. Dilators are easily available online.
A small number will need further counselling.
Vaginitis
Inflammation of the vagina caused by either a simple yeast infection, known as thrush, or bacterial vaginosis.
What can I do about it?
You need either oral or vaginal medication.
If it’s happening often, you may want more whole food plants in your diet.
You need good perineal care hygiene like washing the genital and rectal areas.
Vestibulitis
Inflammation of the vestibular glands located just inside the entrance of the vagina.
What can I do about it?
If treated early, long term vulval and/or vaginal pain may be averted. It usually responds well to:
treatment with local antibiotics
a numbing or soothing agent
steroid ointments to reduce the inflammation.
What else can cause pain?
Physical issues like a very thick hymen, a vaginal band or a thick wall known as a septum can make penetrative intercourse impossible or can result in significant bleeding or vaginal injury.
Women who have been subjected to female genital mutilation may find intercourse painful or impossible and will often need corrective surgery although in some situations vaginal dilators can help.
Cysts and swellings in the vagina such as a Bartholin’s cyst or an abscess but they’re usually short-lived and easily treated medically.
There are also a variety of conditions such as lichen sclerosus, eczema, lichen planus, psoriasis, inflammation of the vestibular glands (vestibulitis) and vulvodynia. The NHS website has a breakdown of each of these.
Psychological reasons for painful sex
Painful sex can arise from past trauma as the mind is intimately related to how your body responds. Here is a non exhaustive list of reasons you may have hesitancy around sex and have pain as a result.
A visit to a gynaecologist or a doctor when you were a small child. If you didn’t feel safe or know what was going on, the negative and long lasting impact can be severe.
Your first smear test.
Your first sexual encounter.
Sexual abuse.
Genital mutilation.
But it’s more nuanced and I often worry about saying it’s psychological because you don’t want to be palmed off by a doctor who says ‘Oh, it’s just in your head’. A lot of pain isn’t picked up yet due to the lack of advances in our collective medical knowledge. Just because we can’t find the cause when we are investigating somebody with pain, it doesn’t mean it’s not there. As doctors, we need to start saying ‘We can’t find a known reason for your pain’ without dismissing it due to our lack of research. Psychological reasons for pain are valid. You are still experiencing pain!
You can find Dr Bajekal on Instagram and TikTok.
She has a tonne of free fact sheets on her website.
She’s written a book! A practical guide to Polycystic Ovary Syndrome (PCOS).
She’s also writing a book on menopause that you can pre order now (it has a whole section on menopause and painful sex!).
What questions would you have liked to have answered? Let us know in the comments and we’ll follow up in a Substack thread very soon!
We’d love it if you’d share this piece with just one other person who you think could benefit from it!